
Spinal Conditions
Condition and Causes
Scoliosis occurs when the spine curves abnormally in one or more places. These curves may affect balance and alignment in the body, and can limit a person’s ability to move normally.
Two percent of people are affected by this deformation of the spine, which frequently develops before puberty. It can be hereditary, or it can occur due to one of several causes:
Secondary: Developed as a reaction to other spinal conditions that change spinal alignment and balance, like degenerative disc disease or osteoporosis. Degenerative adult scoliosis is the term used to describe scoliosis that develops from spinal degeneration.
Congenital: Existing from birth
Myopathic: The muscles around the spine do not work properly due to muscular or neuromuscular disease, like cerebral palsy or muscular dystrophy.
Ideopathic: Arising spontaneously, or from an obscure or unknown cause
Paralytic: The vertebrae in the spine may become unbalanced when the muscles around the spine no longer work due to spinal cord injury
Symptoms and Diagnosis
When scoliosis is present, several signs occur. These include uneven shoulders, shoulder blade protrusion, uneven waist or elevated hip.
A diagnosis can be confirmed using diagnostic tools including X-rays, Computed Tomography (CT) and Magnetic Resonance Imaging (MRI). The Cobb Method can be used to measure the extent a curve has progressed. This method categorizes in terms of degrees. A curve is viewed as significant if it is greater than 25 to 30 degrees. Forty-five to 50 degree curves are viewed as severe and usually require more aggressive treatment.
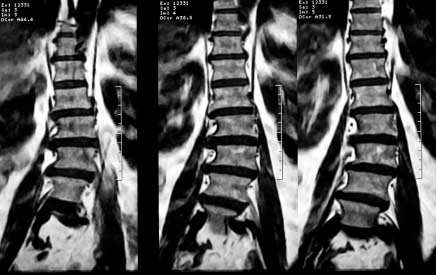 MRI of Degenerative Scoliosis
MRI of Degenerative Scoliosis
Treatment
Most people don’t need treatment. Early detection is important because medical observation can ensure that the curve doesn’t worsen. If intervention is needed, a brace may prevent curvature, but in some cases, spinal fusion surgery made be needed to straighten and stabilize the spine.
Your doctor may consider spinal surgery if the condition hasn’t responded to any other, more conservative treatment, or if your curve advances to more than 40-50 degrees. Other considerations for spinal surgery to treat scoliosis include progressive neurological changes including weakness, tingling or numbness, or if the deformity has become unbearable for physical or aesthetic reasons.
Risks and benefits
Spine surgery to treat scoliosis is a major ordeal for adults. As age advances, the chance of post-surgical complications increases. Spinal stiffening due to degenerative causes can make realignment and correction difficult. If there is osteoporosis in the patient, attaching the instrumentation required for the procedure may be difficult.
Surgical treatment of scoliosis usually aims to:
REMOVE PRESSURE FROM THE SPINAL CORD AND NERVES
REDUCE THE CURVE AS MUCH AS POSSIBLE
STOP THE CURVE FROM PROGRESSING
PROTECT THE NERVES AND SPINAL CORD FROM FURTHER DAMAGE
ALLOW NERVE COMPRESSION TO IMPROVE NEUROLOGICAL FUNCTION OF THE LOWER EXTREMITIES IN OLDER PATIENTS
Failure to take preventive measures for any spinal condition may result in a further aggravated condition. Surgical measures for advanced cases may give relief from extremity pain. The risks involved with surgery are common – infection, blood loss, damage to nerves and spine – and some specific to your treatment. This material is intended to give the patient an overview of surgical procedures and treatments and is not intended to replace the advice and guidance of a physician. Always consult with your doctor about the particular risks and benefits of your treatment.
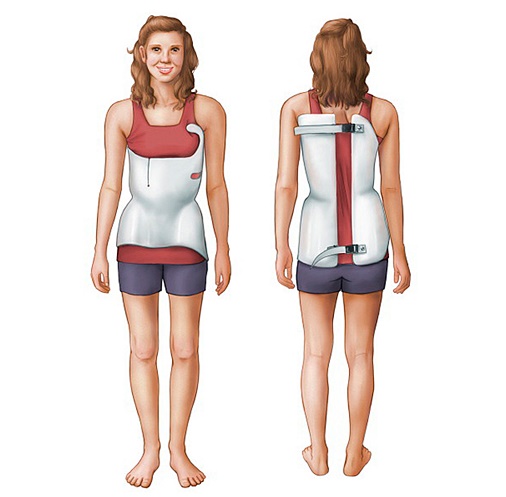
Scoliosis Bracing

Scoliosis Surgical Correction
Kyphosis: excessive curvature of spine; bowing or rounding of the back, can result in a hunchback posture.
Condition and Causes
When viewed from the side, the spine has some normal, gradual curves. The neck and lumbar sections of the spine have a lordotic curve, which means that they curve inward. The thoracic spine has a kyphotic curve, which means that it curves outward. The curves help to keep the body balanced above the pelvis. Kyphosis occurs when a kyphotic curve is excessive and causes a bowing or rounding of the back, which sometimes results in a slouching or hunchback posture. Severe kyphosis can cause pain and serious problems with organs and tissue.
Degenerative diseases, vertebral compression fractures, or trauma to the spine can cause kyphosis. Infections, paralytic disorders, spina bifida, connective tissue disorders, and tumors can also lead to kyphosis. There are several different types of kyphosis, the most common of which is Postural kyphosis. Postural kyphosis occurs when poor posture or slouching stretches ligaments in the spine, leading to abnormal vertebral formation. It creates a smooth curve that is not usually painful or problematic. This type of kyphosis is most commonly found in adolescent girls.
Another type of kyphosis is Scheueremann’s Disease, in which vertebral wedging and reduced intervertebral disc space cause a stiff curve to form in the upper-middle spine. Scheueremann’s Disease is more prevalent in boys and usually begins between 12-15 years of age. It may cause back pain, and some with this disease may also have mild scoliosis.
Congenital kyphosis occurs when the spinal column is irregularly formed during fetal development. Bones may be malformed or vertebrae may be fused together, and the condition may worsen as the child ages. In some cases, congenital kyphosis can lead to lower body paralysis.
Symptoms and Diagnosis
Symptoms of kyphosis include rounded back posture, tenderness or stiffness of the spine, fatigue and mild back pain. In severe cases, a patient may have difficulty breathing.
In order to diagnose kyphosis, a physician will go over the history of a patient’s condition and follow with a physical exam. A forward bend test may be used to observe and confirm the presence of abnormal spine curvature. In order to determine if the excessive curve is caused by bad posture, the physician may ask the patient to lie flat. If there is no deformity when the patient lies on his or her back, the kyphosis is caused by poor posture. If the curve is still present, the kyphosis is caused by structural problems in the spine.
The physician will also test for signs of weakness or changes in sensation below the curve to determine if any changes have taken place in the nervous system.
To confirm the diagnosis, the doctor will take an X-ray to determine the degree of the curve and to find out if there is any vertebral deformity, which can help to identify the type of kyphosis.
Treatment
Treatment for kyphosis ranges depending on the severity and cause of the curve. Other considerations include progression and the age of the patient. Nonsurgical treatments include observation, physical therapy and bracing. Surgery may be needed if the curve is particularly extreme, or if nonsurgical treatments have failed to have an affect on the curve or symptoms after a certain period of time.
Risks and benefits
Failure to take preventive measures for any spinal condition may result in a further aggravated condition. Surgical measures for advanced cases may give relief from extremity pain. The risks involved with surgery are common – infection, blood loss, non-union, damage to nerves and spine – and some specific to your treatment. This material is intended to give the patient an overview of surgical procedures and treatments and is not intended to replace the advice and guidance of a physician. Always consult with your doctor about the particular risks and benefits of your treatment.
There are many different types of spine tumors, which are diagnosed and treated by their location and the type of cells they contain. The experts in our Multidisciplinary Spine Tumor Service have experience in treating all types of spine tumors, even those that are complex and advanced.
Most tumors that begin in the spine or spread from another part of the body are epidural tumors. These tumors grow in the bones of the spine. As they grow, they can compress the spinal cord, nerve roots, and spinal fluid.
Intradural tumors are another type. This group includes:
Intramedullary tumors that grow within the spinal cord, such as ependymomas and astrocytomas
Extramedullary tumors that grow outside the spinal cord, such as meningiomas, schwannomas, and myxopapillary ependymomas
Tumors called nerve plexus tumors grow next to the spine in the nerve plexus. They include such tumors as neurofibromas and ganglioneuromas. Some spine tumors, such as astrocytomas, happen more commonly in children and teenagers.
Spondylolisthesis: one vertebra slips forward; can cause back and leg pain, as well as other symptoms.
Condition and Causes
The spine is made of 33 bones called vertebrae. When one of these bones slips forward on the adjacent neighboring vertebra, this is called spondylolisthesis. This condition can cause back and leg pain, as well as other symptoms. Spondylolisthesis may be hereditary, or it may be the result of stress placed on the spine. It can also be due to spinal degeneration. This condition can gradually cause a deformity of the lower spine, and it can narrow the vertebral canal.
There are five different types of spondylolisthesis:
- Dysplastic spondylolisthesis occurs when a defect in the facet allows the vertebra to slip forward. This type is congenital, meaning the patient is born with it.
- Isthmic spondylolisthesis occurs when there is a defect in a portion of the vertebra called the pars interarticularis. This condition can be caused by repetitive trauma, and it is more evident in athletes who may hyperextend, like football linemen or gymnasts. However, if there is no slippage of a vertebra, the patient has spondylolysis. Isthmic spondylolisthesis can be further divided into three categories:
- Type II A: often called lytic or stress spondylolisthesis, this type is likely caused by repeated micro-fractures due to hyperextension. This type is more common in males and is called a “stress fracture” of the pars interarticularii.
- Type II B: likely also occurs from micro-fractures in the pars interarticularii. This type is different from the preceding type in that the pars interarticularii stay intact, but stretch out as new bone fills in the fractures.
- Type II C: caused by an acute fracture of the pars interarticularii. This type is very rare, and may require nuclear imaging to firmly establish diagnosis.
- Degenerative spondylolisthesis is caused by arthritic changes in the vertebral joints due to cartilage degeneration. This condition is more common in older patients.
- Traumatic spondylolisthesis is caused by injury or direct trauma to the vertebrae. In this type of spondylolisthesis, a fracture of the lamina, pedicle or facet joints lets the front part of the vertebra to slip forward.
- Pathologic spondylolisthesis occurs when the bone is made structurally weak due to a disease, like a tumor or another bone disorder.
Symptoms and diagnosis
Lower back pain is the most common symptom of spondylolisthesis. The pain is often made worse by bending forward and relieved by bending back. The amount of pain experienced does not correlate to the degree to which the vertebra has slipped. Leg pain may also be felt, which may be due to narrowing of the space where the nerves leave the spinal canal.
Half of patients with spondylolisthesis will associate the onset of their symptoms with an injury. Often a patient will lay the groundwork for the injury earlier on in life by developing a lesion. This lesion may not develop into spondylolisthesis until much later in life.
There is usually little deformity detectable, and range of motion is not usually impacted. Often, tightness of the hamstring muscles is the first physical sign of spondylolisthesis. Back pain may occur at irregular intervals, particularly when arching the back. If a nerve is being pinched by spondylolisthesis, a patient may display symptoms similar to those seen with a herniated disc, including muscle weakness of the legs, numbness or tingling in the feet and leg pain.
Treatment
Treatment varies, depending on if the type of slip, the patient’s age and symptoms, and whether pressure is being put on nerves. For those whose nerves are not affected by the vertebral slippage, treatment starts with non-surgical treatments like medication and physical therapy. Bracing may also be recommended. If symptoms are manageable and the slip is small, the treatment will likely be observation. Activity restrictions may be necessary for children, like abstaining from certain sports.
If the slip is more severe or symptoms of nerve compression are present, surgery may be recommended. Surgeries for this condition include spinal decompression, where bone is removed to make room for the nerve being compressed, or spinal fusion. These surgeries are often done at the same time.
Risks and benefits
Failure to take preventive measures for any spinal condition may result in a further aggravated condition. Surgical measures for advanced cases may give relief from extremity pain. The risks involved with surgery are common – infection, blood loss, damage to nerves and spine – and some specific to your treatment. This material is intended to give the patient an overview of surgical procedures and treatments and is not intended to replace the advice and guidance of a physician. Always consult with your doctor about the particular risks and benefits of your treatment.
Cervical
Thoracic
Lumbar
Cervical
Thoracic
Lumbar
Cranial Conditions
Brain Tumor: an abnormal growth that occurs due to uncontrolled cell multiplication often classified by their origin or how they grow
What are Tumors?
A brain tumor is an abnormal growth that occurs due to uncontrolled cell multiplication. The presence of brain tumors can affect the normal structure and activities of the brain in many ways, including increasing pressure on the brain or skull, blocking structures, or damaging nerves and tissue.
Brain tumors are most often classified by their origin or how they grow. Regardless of classification, any brain tumor has the potential to become life-threatening if left untreated.
When classifying by origin, the terms used are Primary and Metastatic.
Primary tumors are those located at the site where the tumor began to grow or originated, meaning primary brain tumors rarely spread to other areas. Primary brain tumors can be further classified as glial tumors and non-glial tumors. Glial tumors are also called gliomas.
Metastatic, or secondary, tumors are those that have spread to other parts of body from the original tumor site.
When classifying by rate of growth, the terms used are Benign and Malignant.
Malignant, or cancerous, tumors tend to keep growing despite treatment and can become life threatening.
Benign, or non-cancerous, tumors tend to grow slower than malignant tumors. Depending on their location in the brain, benign tumors can often be cured by treatment or removal, but they can still cause serious issues if left untreated.
Causes of Brain Tumors
A tumor is an abnormal growth caused by abnormal cell multiplication that does not serve any physiological function. Cell division is regulated by the tumor suppressor genes. These genes also help to repair any damage caused to the DNA. Tumor suppressor genes are constantly at war against the cancer-causing genes called oncogenes. When tumor suppressor genes fail to function properly due to mutations that affect protein encoding, unregulated cell division and growth can occur and cause the development of a tumor.
The body's natural defense system should optimally detect the abnormal cells and kill them. But tumors may produce substances that obstruct the immune system from recognizing the abnormality of tumor cells and eventually the tumor cells may overpower all internal and external checks to their growth.
Certain types of radiation exposure and genetic disorders have been linked with brain tumors. Although some environmental factors are suspected of contributing to the development of tumors, doctors do not know many of the risk factors of many types of tumors yet.
Symptoms of Brain Tumors:
There are many different kinds of brain tumors, so the symptoms will vary depending on the specific type, size, and location of the tumor. Some of the more common symptoms of brain tumors include:
Headaches are one of the most common symptoms of brain tumors. Specifically, headaches upon waking, non-migraine headaches accompanied by vomiting, headaches accompanied by double vision, numbness, or weakness, and headaches accompanied by neck pain.
- Seizure
- Changes in personality or behavior
- Changes in mental function, which could include memory loss, confusion, speech difficulty, or impaired concentration or reasoning
- Increase in sleeping time
- Gradual loss of movement or sensation in arms or legs, balance problems
- Difficulties with speech and comprehension
visual problems or changes
Diagnosis of Tumors
Your doctor will perform a neurological exam to test your mental and physical functioning. During this exam, faculties including your eyes, ears, nose, muscles, sensations, balance, coordination, mental state and memory may be tested. If the results are abnormal, imaging studies may be used to give a clearer image of the brain. Tests performed may include magnetic resonance imaging, or MRI, computed tomography, or CT, and biopsy to examine a sample of tissue from the tumor.
Treatment Options for Brain Tumors
If the tumor is static or growing slowly and does not cause pressure on the adjacent brain tissue, conservative therapy may be utilized. Patients are closely monitored on a regular basis with MRI scans and if the tumor grows or the patient develops symptoms related to it, treatment is started.
If the tumor is growing fast, or is life threatening, definitive therapy may be utilized. This can include more aggressive treatment techniques such as surgery, radiation therapy, or chemotherapy. Biopsies and surgical treatment of brain tumors generally require a craniotomy.
All information provided on this website is for information purposes only. Please see a healthcare professional for medical advice. If you are seeking this information in an emergency situation, please call 911 and seek emergency help.
Chiari Malformation: when part of skull is deformed or too small, which puts pressure on brain and brainstem.
What is a Chiari Malformation?
A Chiari Malformation occurs when the part of the skull that contains the cerebellum is deformed or too small, which puts pressure on the brain and brainstem, forcing it past the opening to the spinal canal. The pressure on the cerebellum can cause signs of neurological problems. Forcing the cerebellum into the upper spinal canal can also disrupt the flow of cerebrospinal fluid, which protects the brain and spinal cord. This can interfere with the signals normally transmitted between the brain and the body. It can also cause spinal fluid to build up in the spinal cord or brain.
What causes Chiari Malformations?
The cause of Chiari malformation is not currently known, but it may be due to problems during fetal development, like exposure to hazardous substances. It may also run in families. There are four types of Chiari malformation:
TYPE I: This is the adult form of chiari malformation, and the most common of the four types. It develops as the brain and skull grow, so symptoms may not appear until adulthood or adolescence. This type does not involve the brainstem.
TYPE II: This type is congenital and is the most common pediatric form of chiari malformation. This type forces the cerebellum and brainstem into the upper spinal canal. Type ii is often seen in infants born with spina bifida, which causes part of the spinal cord and its surrounding structures to form outside the body, often causing complete or partial paralysis. This type is sometimes associated with hydrocephalus, a condition in which too much cerebral spinal fluid is in the brain. This puts further pressure on the inside of the skull, often creating a larger-than-usual appearance.
TYPE III: This type occurs when, in addition to the cerebellum and brain stem being pushed through the spinal canal opening, part of the fourth ventricle, the part of the brain that circulates cerebral spinal fluid and connects upper parts of the brain, is pushed through the opening to the spinal canal. In this type, the back of the brain can protrude out of the back of the skull. This type is very serious and can cause severe neurological defects.
TYPE IV: This type of chiari malformation occurs when the cerebellum fails to develop normally. The cerebellum may have parts missing or be found further down the spinal canal.
Symptoms and Diagnosis
Symptoms of Chiari malformation Type I typically include headaches that are made worse by coughing, straining or sneezing. Neck pain that sometimes goes down the shoulders and problems with gait and balance also may occur. A patient with Chiari malformation Type I may also have numbness and tingling of the feet and hands, as well as problems with fine motor skills. Slurred speech, vision problems, difficulty swallowing and dizziness are also symptoms. Sometimes, tinnitus, bladder control problems, and sleep apnea can also occur, as well as chest pain and spinal curvature.
In a patient with Chiari malformation Type II, symptoms related to spina bifida may be present. In this type, more tissue is forced into the spinal canal than in Type I.
In Types II, III, and IV, the diagnosis may be made when the patient is born, as the congenital defects will be obvious from birth. A patient with Chiari malformation Type I may not have any symptoms until adolescence or adulthood, so the physician will go over the patient's medical history, asking about developmental milestones and family medical problems. A physical exam will follow, during which the circumference of the head may be measured, and the back may be examined. Diagnostic tests like an MRI or a CT scan can confirm the diagnosis.
How are Chiari Malformations treated?
If the patient is without symptoms or the symptoms are not severe, the physician may prescribe observation and medication. However, to treat severe Chiari malformation, surgery is required to stop the progression of anatomical changes in the brain and spinal canal and to ease symptoms. Surgeries are usually decompressive in nature and may include a spinal laminectomy or a posterior fossa craniectomy. More than one surgery may be needed to treat Chiari malformation.
Risks and benefits
Failure to take preventive measures for any spinal condition may result in a further aggravated condition. Surgical measures for advanced cases may give relief from extremity pain. The risks involved with surgery are common - infection, blood loss, non-union, damage to nerves and spine - and some specific to your treatment. This material is intended to give the patient an overview of surgical procedures and treatments and is not intended to replace the advice and guidance of a physician. Always consult with your doctor about the particular risks and benefits of your treatment.
Meningioma: type of brain tumor, often benign. Some symptoms: headaches, seizures, vision and hearing problems.
What is Meningioma?
Meninges are the three membrane layers that envelop the brain and spinal cord. The (outermost) of these thin layers is the dura mater, the second layer is the arachnoid, and the third layer is the pia mater.
A meningioma is a primary intracranial tumor of the meninges. Primary means that this type of brain tumor develops and stays in the brain. Meningiomas are classified into three grades. Meningiomas are also usually benign, meaning that they grow slowly, but if they are not discovered on a timely basis, they can interfere with the brain's normal functioning. In certain locations, they can be severely disabling and even life threatening if they become large enough. Usually patients develop only a single meningioma; however, several meningiomas may simultaneously grow in other parts of the brain or spinal cord.
Grade 1 is Benign Meningioma, which has the lowest rate of growth and recurrence risk. Grade 2 is Atypical Meningioma, which is more aggressive in terms of growth and recurrence risk. Grade 3 is Malignant (Anaplastic) Meningioma, which has the most aggressive rate of grow and highest risk of recurring.
Cause of Meningiomas
A tumor is an abnormal growth caused by abnormal cell multiplication that does not serve any physiological function. Cell division is regulated by the tumor suppressor genes. These genes also help to repair any damage caused to the DNA. Tumor suppressor genes are constantly at war against the cancer-causing genes called oncogenes. When tumor suppressor genes fail to function properly due to mutations that affect protein encoding, unregulated cell division and growth can occur and cause the development of a tumor.
The body's natural defense system should optimally detect the abnormal cells and kill them. But tumors may produce substances that obstruct the immune system from recognizing the abnormality of tumor cells and eventually the tumor cells may overpower all internal and external checks to their growth.
Certain types of radiation exposure and genetic disorders have been linked with meningiomas. Although some environmental factors are suspected of contributing to the development of tumors, doctors do not know many of the risk factors of many types of tumors yet.
Symptoms of Meningiomas
The symptoms of meningiomas usually become noticeable only when the tumor has grown quite large. Symptoms do not show up in the early stages due to the benign nature of this tumor. Some meningiomas may never exhibit symptoms during a patient's lifetime. Symptoms will vary depending on the size and location of the tumor.
Some common symptoms of meningiomas may include:
- headaches
- seizures
- changes in behavior or personality
- progressive focal neurologic deficit
- confusion and lack of judgment
- nausea and vomiting
- changes in vision
Diagnosis of Meningioma
Since meningiomas may not exhibit any symptoms, they might be detected unexpectedly when a patient has a brain scan for unrelated symptoms.
If a person is suspected of having a meningioma, a neurological exam will be done. This involves checking the function of eyes, ears, nose, and muscles. Sensation, balance and coordination are also tested. Mental state and memory are also assessed.
Diagnostic imaging tests may be ordered, including computerized tomography, or CT, scans or magnetic resonance imaging, or MRI, scans. The results from these imaging studies can help to determine the size, location, and type of tumor. The diagnosis may also be confirmed by examining a tissue sample taken from the tumor in a procedure called a biopsy.
Treatment Options
Observation and less invasive treatment options may be chosen if:
- the symptoms are mild with little or no swelling
- the patient is older and symptoms are increasing slowly
- the other treatment options carry significant risks for the patient
- the symptoms have little effect on the patient's quality of life
Surgery is generally the standard treatment option for meningiomas. Surgery is often successful in treating meningiomas because they are a benign tumor with defined boundaries.
Surgery involves removal of the affected cells. Surgery is scheduled soon after the initial diagnosis. Surgery may not be the only treatment. It is often complemented with other techniques, like radiation therapy if complete removal of all affected cells is not possible or if the tumor is recurrent.

